Weiyi Peng Awarded $1M and $250,000 Grants to Apply Immune Therapy Research
To most people, cancer and Parkinson’s disease have little in common, but to sufferers of the diseases, they both have the ability to upend a person’s life and cause a lifetime of pain.
Scientifically, both diseases contain immune dysfunctions. University of Houston’s Dr. Weiyi Peng, an assistant professor of biology and biochemistry and UH’s Center for Nuclear Receptors and Cell Signaling, is part of a group of cancer and Parkinson’s research experts investigating whether the diseases are caused by similar gene alterations.
Specifically, the group is looking at why changes in the LRRK2 and Parkin genes can cause Parkinson’s and cancer. Peng, both an M.D. and Ph.D., is part of a national group who received nearly $6 million from Aligning Science Across Parkinson’s to study the similar pathogenesis of the two diseases. UH will be receiving about $1M of grant funds.
Peng explains the group saw that the diseases’ common genetic alterations lead to both neurodegeneration and oncogenesis, causing Parkinson’s and cancer, respectively.
Her group in the College of Natural Sciences and Mathematics will provide immunology expertise that could eventually help develop new, immune-based therapies for Parkinson’s.
“My team is particularly focused on generating new clinical models,” Peng said, “which can represent or mirror Parkinson’s disease. And we are studying how the immune system contributes to Parkinson’s disease development.”
New Targets for Cancer Immunotherapy
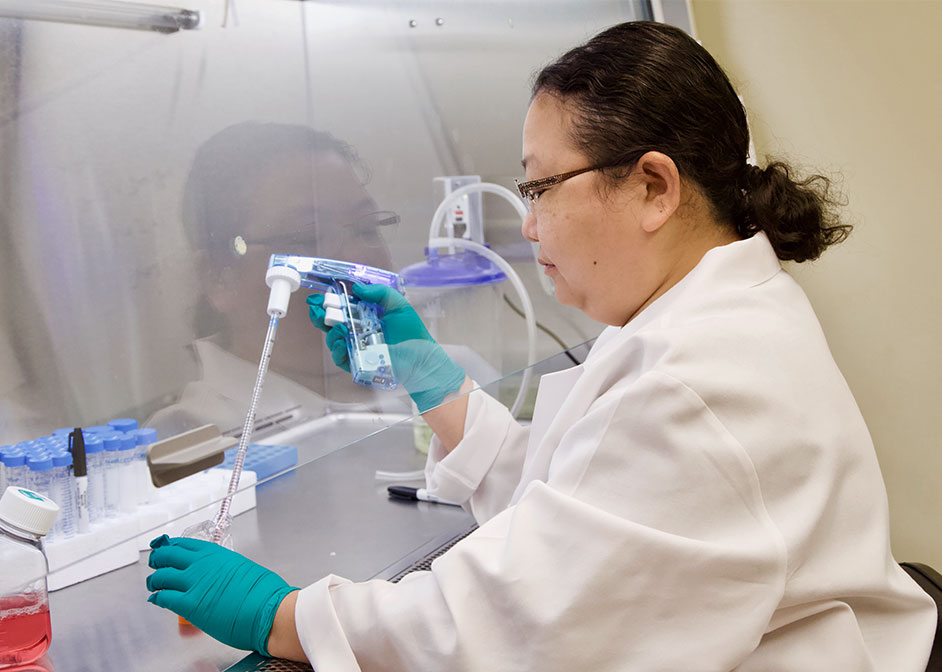
Peng also received a $250,000 grant from the Cancer Prevention & Research Institute of Texas to identify new targets for cancer immunotherapy.
Past immunotherapies have produced positive responses in patients with tumor malignancies. To continue the benefit of immunotherapy for cancer patients, Peng explains it is important for scientists to understand why some cancer patients do not respond to this sort of therapy.
Peng plans to develop a new genetic screening platform by combining an immune platform she created with a single-cell RNA sequencing technology.
Successful results from the project will provide a tool to quickly screen genes and find out whether they will sensitize tumors to immunotherapy. It could also provide researchers a better understanding of immune evasion among the non-responders to cancer immunotherapy.
“This will be the first time we generate this method to address immune resistance mechanisms in cancer patients,” Peng explains. “We could potentially find new targets to improve the efficacy of immune therapy through our new tools.”
New Approaches to Treat Chronic Diseases
Working as a medical doctor, she said she felt we had limited strategies to treat chronic diseases, including cancer.
Around 2000, she realized immunotherapy is an open field, “and has the potential for good.” At the time, cancer treatments focused on chemotherapy, surgery and radiotherapies.
“Cancer immunotherapy is now starting to become the frontline of cancer treatments,” Peng adds. “I’m happy that when I was trying to choose which career path to take, I chose the right angle – immunotherapy.”
Both grants could provide new targets and avenues for Parkinson’s disease or cancer treatment.
“Chronic diseases are very complicated,” she said. “They require multi-disciplinary study and collaborations.”
- Rebeca Trejo, College of Natural Sciences and Mathematics