Best known for its association with the BRCA gene mutations, triple-negative breast
cancer (TNBC) is the only type of breast cancer for which there has yet to be a specific
therapy. This type of cancer generally occurs in younger women, is highly metastatic
and has a very poor prognosis. Researchers at the University of Houston (UH) are taking
on TNBC, hoping their work will lead to new therapies for this devastating disease.
Working with the protein Maternal Embryonic Leucine-Zipper Kinase (MELK), which has
been found to play a role in cancer, the UH research team is working to inactivate
MELK in breast cancer cells in order to observe the effects it has on TNBC cells.
By identifying changed functions and affected proteins, they recently have come to
some conclusions about how MELK affects cells.
“It’s been shown that MELK is in its highest concentrations during cell division,”
said UH biology senior Marisa Simon, who received an undergraduate research fellowship
this summer to work on this project. “My hypothesis is that MELK safeguards cellular
division by blocking the possibility of cell death. This blocking of cell death also
can contribute to the longevity of cells. This gives researchers a potential target
for cancer therapy. If MELK is essential to the division of cancer cells, then inhibiting
it could inhibit and decrease tumor formation. Knowing what is affected by inactivating
MELK will help researchers identify not only whether inhibiting it is effective, but
also if it is safe.”
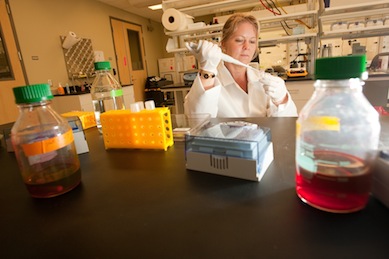
Collaborating with graduate student Fahmi Mesmar and led by assistant professor Cecilia
Williams in UH’s Center for Nuclear Receptors and Cell Signaling (CNRCS), Simon says
they have defined which other proteins and pathways MELK affects in TNBC cells, many
of which relate to the death of cells and the cell cycle. The team is currently working
on confirming these findings.
“Marisa has collected impressive amounts of interesting data,” Williams said. “The
microarray analysis she performed, whereby she analyzed the effect MELK has on every
single gene in our genome’s approximately 23,000 genes, has given us data for the
impact of MELK on a global genome level. We are now working to decipher its impact
to get a wide and complete understanding of what MELK does in TNBC cells, as well
as how we can best use MELK to design better treatments.”
Found in both men and women, the MELK protein also may play a role in other cancers,
such as prostate cancer. The researchers say MELK concentrations are high in stem
cells and appear to protect them from dying. If MELK turns out to be a desirable target
for cancer treatment, then inactivating it could be less hazardous to patients than
conventional chemotherapy and radiation, which have pervasive effects on the body
since they not only target cancer cells, but also other cells within the range of
treatment. Since MELK inhibition would only be targeting the growth of stem cells,
it would decrease these negative impacts. 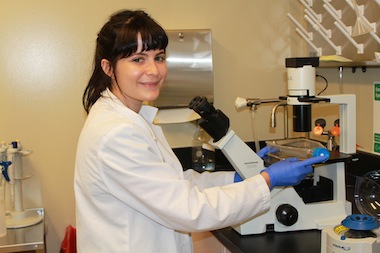
Williams says this research was initiated several years back in her lab, and research
leading up to it has been published in the scientific journals Breast Cancer Research
and Carcinogenesis. Her lab also has several other projects that relate to designing
better treatments for breast cancer, including achieving a better understanding of
how estrogen affects the development and growth of breast cancer and how certain microRNAs
affect metastasis of breast cancer. These studies are connected to a large NIH-funded
project the lab is doing on colon cancer, where estrogen and microRNAs also play a
role and may be used to create better preventative treatments.
“Marisa has been a very good addition to my lab. She is full of enthusiasm, eager
to do the work and has contributed to the direction of the project,” Williams said.
“Her work is extremely relevant to my research of how poor-prognosis breast cancer
functions, so that we can better understand how to target this type of cancer in the
future.”
With her funding being extended to cover her senior honors thesis, Simon recently
presented the research on MELK’s role in TNBC at UH’s annual Undergraduate Research
Day in October. One of UH’s most prolific cancer researchers, Williams’ breast cancer
research is funded, in part, by a grant to the CNRCS from the Texas Emerging Technology
Fund.
###
About the University of Houston
The University of Houston is a Carnegie-designated Tier One public research university
recognized by The Princeton Review as one of the nation’s best colleges for undergraduate
education. UH serves the globally competitive Houston and Gulf Coast Region by providing
world-class faculty, experiential learning and strategic industry partnerships. Located
in the nation’s fourth-largest city, UH serves more than 39,500 students in the most
ethnically and culturally diverse region in the country. For more information about
UH, visit the university’s newsroom.
About the College of Natural Sciences and Mathematics
The UH College of Natural Sciences and Mathematics, with 193 ranked faculty and nearly 6,000 students, offers bachelor’s, master’s and
doctoral degrees in the natural sciences, computational sciences and mathematics.
Faculty members in the departments of biology and biochemistry, chemistry, computer
science, earth and atmospheric sciences, mathematics and physics conduct internationally
recognized research in collaboration with industry, Texas Medical Center institutions,
NASA and others worldwide.
About the UH Center for Nuclear Receptors and Cell Signaling
Established in 2009, UH’s Center for Nuclear Receptors and Cell Signaling (CNRCS) is a leading component of the UH Health initiative. Led by Jan-Åke Gustafsson,
a National Academy of Sciences member and world-renowned expert in the field of nuclear
receptors, CNRCS researchers are involved in many aspects of nuclear receptor research,
all focused on understanding the roles of these receptors in health and disease. CNRCS
researchers are working toward the goal of finding new treatments for an array of
significant diseases including cancer, diabetes, metabolic syndrome and neurological
disorders. Working from the center’s world-class labs, the researchers combine interdisciplinary
research and dynamic collaboration with the Texas Medical Center and industry partners.
To receive UH science news via email, sign up for UH-SciNews.
For additional news alerts about UH, follow us on Facebook and Twitter.